Purplish-red bumps and blisters are seen on. Physicians should also be aware of the potential for misdiagnosis especially in light of the.

Covid 19 Skin Rash Website Criticised For Lack Of Bame Examples Coronavirus The Guardian
If youre on the lookout for symptoms of COVID-19 youre likely watching for a dry cough fever and shortness of breath.

Is a neck rash a symptom of covid. There is a high chance of misdiagnosis due to lack of supportive. Until more information is found on skin rashes as a symptom of covid there is no strong support whether to take a skin rash patient for a covid test or not. Purplish raised areas on the fingers is quite a specific rash for COVID and is usually painful.
Jessica Bortz Schaap developed a rash on her neck months after her COVID-19 symptoms arrived. Although there are reports of otolaryngological symptoms and manifestations of CoronaVirus Disease 19 COVID-19 there have been no documented cases of sudden neck swelling with rash in patients with Severe Acute Respiratory Syndrome Coronavirus 2 SARS-CoV-2 infection described in literature. The symptom has emerged in research studies of COVID-19 patients and as more is learned about the.
COVID can come with a range of symptoms from the severe like shortness of breath to symptoms that disguise themselves as the common cold and in some cases patients have no symptoms at all. A skin rash is a possible symptom of COVID-19. And for one in five people 21 who reported a rash and were confirmed as being infected with coronavirus the rash was their only symptom.
Three types of rashes are identified in the research by Kings College London leading those behind the study to call for skin rashes to be included as a fourth key symptom of COVID-19. Like other coronaviruses SARS-Cov-2 infiltrates the body by attaching to a receptor ACE2 found on some cells. A rash can also be a sign of another disease.
It can also cause multiple red and sore bumps on many fingers and it may be difficult to type. If youd broken out in a rash this time last year itd be safe to assume it was from a new lotion you had used a. If you develop a rash tell your doctor A rash may be a sign of COVID-19.
The rashes associated with COVID-19. The Covid Symptom Study app revealed that around 9 of coronavirus patients reported a body rash or a rash on their fingers or toes while rashes were twice as common in children. Rash is one of the less common symptoms of COVID-19.
There are other less common rashes associated with COVID-19 including Pityriasis Rosea-like light-sensitive rashes affecting the face or neck. But one of the oddest aspects of COVID has been its effect on the skin. Vasculitis rashes when small blood vessels in the skin become damaged are also seen in severe.
A skin rash can sometimes be the only symptom of people infected with COVID-19 a study has concluded. It can take on many forms including hives macules papules or a toe rash. 17 of respondents testing positive for coronavirus reported a rash as the first symptom of the disease.
There is no confirmed way to determine whether a skin rash is caused by covid-19 or due to some other underlying disease unless you have other covid symptoms as well. The NHS say the disorder is a painful swelling of the thyroid gland thought to be triggered by a viral infection such as mumps or the flu. Watch for Rash Until more is known clinicians should be aware that a rash may be a symptom of COVID-19 and know that skin symptoms in addition to other clinical clues may be used to support a diagnosis or as a factor in deciding whether or not to recommend a patient be tested for the disease.
COVID can come with a range of symptoms from the severe like shortness of breath to symptoms that disguise themselves as the common cold and in some cases patients have no symptoms at all. Its unknown what exactly causes COVID-19. When the rash recovers the top layers of the skin may peel where the purplish bumps were.
The three established symptoms of COVID-19 as recognised by the NHS are a high temperature a new.
In the past just minutes after getting the influenza vaccine she had hives wheezing and throat swelling. If You Are Allergic to an Ingredient in a COVID-19 Vaccine.

A Guide To Who Can Safely Get The Pfizer Biontech Covid 19 Vaccine
If you have had a severe allergic reaction or an immediate allergic reactioneven if it was not severeto any ingredient in an mRNA COVID-19 vaccine you should not get either of the currently available mRNA COVID-19 vaccines Pfizer-BioNTech and Moderna.

Allergic to flu shot is covid vaccine safe. Contrary to the claims that COVID-19 vaccines caused hundreds of deaths none of the reported deaths has been attributed to the vaccine. There is no evidence that people with allergic conditions such as asthma hay fever food allergy or insect sting allergy are at any greater risk of vaccine allergy compared to the general population. Lets start with the flu vaccine.
Severe allergic reactions to COVID-19 vaccines. Although each vaccine targets a virus that causes a respiratory illness they use different mechanisms to prime the bodys immune response. There were 85 reported deaths following influenza vaccination in 2017.
The intensive care unit nurse was worried the COVID-19 vaccine would kill her. The vaccine against the coronavirus that causes COVID-19 is not the same as the influenza vaccine. The Centers for Disease Control and Prevention on Sunday said people who have.
Allergic reactions arent a unique side effect of the COVID-19 vaccine Brown says. Its recommended that if youve had an allergic reaction any of the ingredients in the vaccine you should not get it. Several infectious disease experts say that the logic behind these concerns is mistaken.
119 deaths in 2018. Murphy answers viewer COVID-19 questions 910. COVID-19 vaccines are safe for people with severe allergies.
The Pfizer and AstraZeneca vaccines are both safe for people with allergies. Its important to obtain the flu vaccine even if you have received the COVID vaccine. Many common side effects of vaccination such as localised pain and swelling at the site of injection or flu-like symptoms can be mistaken for allergy.
But the CDC says that you should avoid any particular vaccine. And 203 deaths in 2019. Safety monitoring indicates that COVID-19 vaccines are generally safe and effective and mostly cause mild side effects.
CDC says people with history of severe allergic reactions can get COVID-19 vaccine. People who are allergic to eggs sometimes have an. The PfizerBioNTech and Moderna vaccines.
Are COVID-19 vaccines safe for people with allergies. People respond adversely to many vaccines including the flu vaccine which is incubated in chicken eggs for example. Between mid-December 2020 and April 23 2021 at which point between 95 million and 100 million Americans had received their COVID-19 shots there were 3544 reported deaths following COVID vaccination or about 30 per day.
This is what is known as an inactivated vaccine. Yes the viruses are different and so are the vaccines. June 16 2021 -- Giving a COVID-19 vaccine at the same time as a seasonal flu vaccine appears safe and effective according to a new study.
If Im allergic to the flu shot could I have the same reaction to the COVID-19 vaccine Dr. In the US reasons for vaccine hesitancy run the gamut ranging from possible side effects to distrust in the government. Health Dec 14 2020 215 PM EDT.
The US Food and Drug Administration FDA is not recommending that anyone with allergies avoid COVID-19 vaccination categorically. But overall having allergies doesnt exclude you from getting the vaccine. Neither will protect from the other.
They are not a reason to avoid the PfizerBioNTech or AstraZeneca COVID-19 vaccine or Moderna vaccine. Centers for Disease Control and Prevention has reported that allergic reactions to the COVID-19 vaccine can occur but they are rare. Is it safe for people allergic to penicillin or who have had reactions to shots or skin reactions to nickel to get the vaccineANSWER.
Additionally some people have questioned why they would need to get a COVID-19 vaccine if they normally dont get the flu shot. If you had an allergic reaction to the first dose of a COVID-19 vaccine the CDC doesnt recommend getting the second dose. It is very safe for them to do that Levine said.
Chinese scientists have conducted some early research with rhesus monkeys and found that antibodies after recovery from COVID-19 protected. We are hopeful that a similar pattern of responses lasting over time will also emerge for the vaccine.

Could Efforts To Fight The Coronavirus Lead To Overuse Of Antibiotics The Pew Charitable Trusts
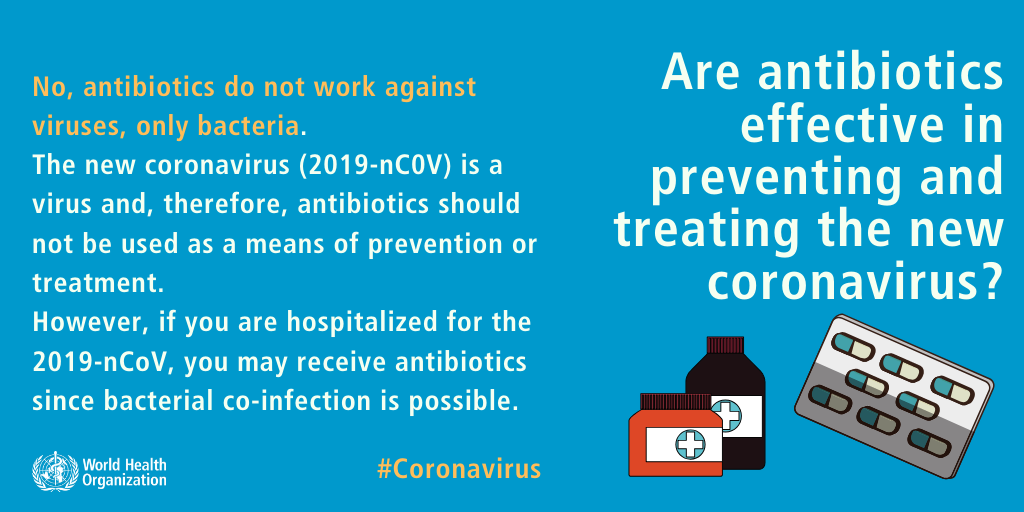
Azithromycin Zithromax is a macrolide antibiotic that is being investigated as a potential treatment for people with COVID-19 the disease caused by the new coronavirus SARS-CoV-2.
How long do antibiotics stay in your system after covid. The virus uses this protein to enter cells. The study found that mild cases of COVID result in lasting antibody protection and that reinfections are likely uncommon. The number and type of antibodies varied between people.
While normally a COVID-19 patient for the most part takes 3 weeks to recover new researches have called attention towards those individuals. They slightly decreased six to eight months. But the levels usually remained stable over time.
A period of seven full days since symptoms first appeared. Of the people who recovered 95 had immune system memories of the virus that causes COVID-19 SARS-CoV-2. Because of this antibody tests should not be used to.
If you do start to develop symptoms you should isolate for at least 10 days. Almost everyone had antibodies that block the virus spike protein. Even people who did not have COVID-19 symptoms in the days or weeks after they were infected can have post-COVID.
So while its impossible to say. People should stay away from others for 10 days after symptoms first appear. Its very important to realize that we do not need to give antibiotics to patients who are isolated with COVID-19 in their homes because they have mild disease.
In humans Berezow notes that changes to gut flora or the bacteria living within your digestive tract can also make you more susceptible to infection. However 95 of the people had at least 3 out of 5 immune-system components that could recognize SARS-CoV-2 up to 8 months after infection. Antibodies can take several days or weeks to develop after you have an infection and may stay in your blood for several weeks after recovery.
Experts also dont have information about the outcome of every infection. The final measurements were taken at a mean of 86 days after the onset of symptoms ranging from 44 to 119 days. Some studies suggest antibodies disappear as quickly as two months later but these latest findings out of Canada agree with the leading American immunologists.
And the changes to the important microorganisms in your gut due to antibiotics can be permanent. If you never have symptoms the 10-day window starts after you get a positive result on a COVID-19 test. There is currently no evidence the virus can survive in food but early evidence suggests it may last several hours on copper 24 hours on cardboard and up to 72 hours on plastic and steel.
Read on to find out what you should hold off on for 48 hours after your shot and for more on vaccines check out The CDC Says You Should Immediately Do This Once Youve Been Vaccinated. In the UK the NHS recommends 7 days after symptoms emerge continuing if symptoms persist. However early estimates predict that the overall COVID-19 recovery rate is between 97 and 9975.
Several months ago our studies showed that natural infection induced a strong response and this study now shows that the responses last Weiskopf says. They must also continue quarantining for. Although most people with COVID-19 get better within weeks of illness some people experience post-COVID conditions.
CDC currently recommends COVID-19 cases isolate for 10 days after they start feeling ill and three days after their fever dissipates. Post-COVID conditions are a wide range of new returning or ongoing health problems people can experience four or more weeks after first being infected with the virus that causes COVID-19. Your normal flora may never actually return completely to normal Berezow says.
People who have COVID-19 or think that they have COVID-19. The CDC defines recovery from COVID-19 as an absence of fever with no use of fever-reducing medication for three full days. It turns out according to the experts some behavior is best to avoid in the aftermath of your vaccine lest you want to feel worse.
While the study found antibody-producing cells in people 11 months after they experienced their first symptoms researchers believe immunity lasts even longer than. The antibodies they found had a half-life of 73 days. And to only be receiving antibiotics if they are significantly ill where the healthcare provider is suspicious of on top of the COVID-19 the patient having a bacterial infection.
It is already used for the treatment of community-acquired pneumonia caused by designated susceptible bacteria and for the treatment of other bacterial infections. Improvement in other symptoms such as coughing and shortness of breath. That means that half of the antibodies would be gone at 73 days.
Other cases were more recent. At that point if your symptoms have improved and youve been without a fever for at least 24 hours it should be safe. New research shows that the antibodies that develop from COVID-19 remain in the body for at least 8 months.
How You Might Feel.
If there is a high risk of an allergic reaction to one of the vaccines eg. If you have a serious allergic reaction to the 1st dose of a vaccine you should not have the same vaccine for your 2nd dose.

Covid 19 Vaccines And Allergies Anaphylaxis Campaign
The COVID-19 vaccines currently available are given in 2 doses.

Can i have the covid vaccine if i am allergic to penicillin nhs. The good doctor asked if I had any history of allergic reactions to penicillin. Penicillin does not form part of the PfizerBioNtech vaccine. People with penicillin allergies have been told they can have the Pfizer vaccine or any other Covid-19 vaccine.
The only person who has a significant contrary indication to the current mRNA vaccines are those who have allergies to. Its recommended that if youve had an allergic reaction any of the ingredients in the vaccine you should not get it. According to the Anaphylaxis Campaign people with a penicillin allergy can have the vaccine.
If you have a history of immediate onset anaphylaxis to multiple classes of drugs or unexplained anaphylaxis please also refer to the additional information at. People with a history of significant allergic reactions should not receive the Covid vaccine the medicines regulator has said after two NHS workers experienced symptoms on. If You Are Allergic to an Ingredient in a COVID-19 Vaccine If you have had a severe allergic reaction or an immediate allergic reactioneven if it was not severeto any ingredient in an mRNA COVID-19 vaccine you should not get either of the currently available mRNA COVID-19 vaccines Pfizer-BioNTech and Moderna.
If youre aged 18 or over or will turn 18 within 3 months you can. Known allergy to PEG or Polysorbate 80 it may be possible to have another vaccine which does not contain the ingredient subject to availability and. Those with a penicillin allergy may fear not however.
Penicillin does not form part of the PfizerBioNtech vaccine. However a vaccine works through stimulating your immune system. It is very safe for them to do that Levine said.
The Sun Online has contacted the MHRA for clarification on whether those with penicillin allergies are excluded from having the Covid jab. However a vaccine works through stimulating your immune system. Back in early December use of the Pfizer vaccine in people with a history of severe allergies was paused in the UK after two NHS workers who both had a history of allergies suffered a mild reaction to the vaccine.
Last year I took my first penicillin vaccine. Anaphylaxis with one type of COVID-19 vaccine may not preclude vaccination with another vaccine but this should only occur if the precautions listed above are met. Serious allergic reactions to the COVID-19 vaccines are very rare.
Dr Thompson added. Staff giving the vaccine are trained to deal with allergic reactions and treat them immediately. The organisation states people who.
The health workers who are understood to both have a history of. Book your COVID-19 vaccination appointments online for an appointment at a vaccination centre or. Guidance for the vaccine was altered after two NHS staff members who received the jab last month had allergic reactions.
You usually have the 2nd dose 8 to 12 weeks after the 1st dose. I cant say because I am a penicillin virgin. Yes allergy to penicillins is not a contraindication to the PfizerBioNTech or AstraZeneca COVID-19 vaccine or Moderna vaccine.
If you do have a reaction it usually happens in minutes. Guidance for the vaccine was altered after two NHS staff members who received the jab last month had allergic reactions. Having a food allergy is not a contraindication to receiving any of the currently approved UK COVID-19 vaccinations and it is important that all people including individuals with food allergies have the correct and most up to date information to ensure they.
Dr Thompson added. The MHRA has warned that those with severe allergic reactions such as a severe penicillin allergy may be at risk of having an allergic response to the vaccine. If you had an allergic reaction to the first dose of a COVID-19 vaccine the CDC doesnt recommend getting the second dose.
But overall having allergies doesnt exclude you from getting the vaccine.
Disturbingly all these different mechanisms of harm have synergistic effects when it comes to dysregulating your innate and adaptive immune systems and activating latent virusesThe worst symptoms of COVID-19 are created by the SARS-CoV-2 spike protein and that is the very thing. A 2004 study of individuals who were vaccinated against measles as children found strong T-cell immunity more than 30 years later.

No Vaccine Side Effects Don T Tell You How Well Your Immune System Will Protect You From Covid 19
We dont know how long T-cell immunity persists after COVID-19 vaccination or infection but theres evidence that T cells last for quite a while.

How long does a covid shot last in your system. 3D image of tomography datas displaying Covid-19 symptoms on lungs and the overall damage of the virus to the body at a state hospital in Moscow Russia on May 22 2020. This suggests that for some people COVID-19 symptoms last longer than original estimates even in mild cases. How Long Does The COVID-19 Booster Shot Last.
One is that the three coronavirus vaccines authorized for use in the United States provide a high degree of protection for at least three months based on clinical trials that began as early as last. Studies of recovered COVID-19 patients and vaccine recipients show that immunity to the coronavirus may last anywhere from 6 months to a year or more. COVID-19 vaccines are capable of causing damage in a number of different ways.
Get all the facts at GoodRx. The immune system quickly identifies attacks and destroys the spike proteins because it recognizes them as not part of you. Moderate or severe primary immunodeficiency such as.
Received a stem cell transplant within the last two years or are taking medicine to suppress the immune system. 11 2021 in Long Beach Calif. Johnson Johnsons Jansen JJJanssen COVID-19 vaccine requires only one dose.
A piece of the answer came last week from Pfizer which announced that antibodies triggered by the jab and the strong immunity they prompt persists for. The COVID-19 recovery period depends on the severity of the illness. By comparison over 90 of people with influenza or flu recover within.
After the protein is made the cells break down those instructions and your body gets rid of it. 3 This was true for mild and severe cases though people with severe disease ended up with more antibodies overall. Aug 22 2021 - Health Digest.
A new study suggests that the efficacy of PfizerBioNTech COVID-19 vaccine gradually declines in the six months after administration likely due to the delta variant. According to new research from Pfizer and Moderna it looks like COVID-19 immunity will last at least six months in fully vaccinated people though studies are ongoing. If you have a mild case you can expect to recover within about two weeks.
However your second dose may be given up to 6 weeks 42 days after the first dose if necessary. According to the CDC full protection occurs two weeks after the second dose of the Pfizer-BioNTech or Moderna COVID-19 vaccines or two weeks after the single-dose Johnson Johnson vaccine. One study published in the journal Immunity of 5882 people who had recovered from covid-19 infection found that antibodies were still present in their blood five to seven months after illness.
In the meantime there are a few things we do know. Experts dont yet know how long a booster shot will last but are recommending to get them eight months after your final previous vaccination shot. A nurse administers a dose of the Pfizer COVID-19 vaccine to a college student at the California State University Long Beach campus on Aug.
The Infectious Disease Society of America IDSA estimates that the spike proteins that were generated by COVID-19 vaccines last up to a few weeks like other proteins made by the body. In December Moderna published a study that showed their COVID-19 vaccine still showed good immune responses four months after the date of vaccination results which Professor Triccas said were encouraging. If you receive a vaccine that requires two doses you should get your second shot as close to the recommended interval as possible.
After receiving a COVID-19 vaccine it takes weeks for your immunity to build. Reese-Willis said the vaccine does not stay in our system forever but that once the code sends the genetic instructions to your immune cells the cells create a protein piece that then gives the immune system the ability to fight off the virus. Thats the best Ive seen in terms of how far theyve measured out he said.